Macula lutea is a circular area oriented in the central retina. Retina is the inner, neural tissue of the eye, where the light is transformed in electrical signal and is transmitted through the optic nerve to the brain. Macula is responsible for central vision and recognition of faces and color vision. Any disorder on this area causes central vision damage.
Age Related Macular Degeneration and central vision
Age related macular degeneration (AMD) influences the macula, causing damage of the central, sharp vision. Central vision is important for reading, driving and other daily activities. In some cases the AMD progresses so slowly that patients observe minimal change in their vision, while in other cases the disease progresses more quickly and may result in loss of central vision in both eyes. AMD is a leading cause for vision loss in people over 60 years old and may occur in two types: dry and wet AMD.
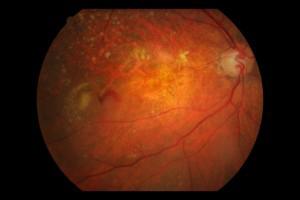
Wet Age Related Macular Degeneration
Wet AMD causes loss of central vision within a few days. The characteristic of this type is the formation of new pathological vessels on the macula. These vessels are very fragile and often there is blood or fluid leakage. As a result, the macula is lifted from its normal position in the back of the eye. In wet AMD, macular damage occurs very quickly.
 Age Related Macular Degeneration: Wet type
Age Related Macular Degeneration: Wet type
An early symptom of wet AMD is the straight lines, which appear wavy. If anyone notice such changes in his vision, he should contact to an ophthalmologist for a fundus examination under dilated pupils.
Dry Age Related Macular Degeneration
Dry AMD occurs when macular light-sensitive cells are slowly destroyed, so that the vision is gradually decreased. As the condition becomes worse, patients may notice a blurred spot in their central field of view. Over time, macula loses its function, so the central vision is lost in the affected eyes.

The most common symptom of dry AMD is the blurred central vision. There may be also difficulty in recognizing faces, or maybe there is more need of good light conditions when reading or in other activities. Dry AMD usually affects both eyes, but vision loss precedes in one eye. Characteristic finding on fundoscopy is the appearance of drusen.
Drusen characteristics
Drusens are yellow-type deposits, which are located under the retina. There are seen often in people over 60 years old. The ophthalmologist may notice the drusens through fundoscopy (examination through dilated pupils).
Drusens do not cause vision loss by themselves. In fact, scientists are not sure about the exact connection of drusens with AMD, but it is certain that an increase in the number and size of drusens, increases the patient's risk of developing AMD.
 Fundus photo showing drusen in dry AMD
Fundus photo showing drusen in dry AMD
The three steps of dry Age Related Macular Degeneration
The dry type of AMD is composed by three steps, which may occur either in one eye or in both eyes.
1. Early dry AMD
At this stage people may have many small drusens without having symptoms or vision loss.
2. Intermediate dry AMD
People at this stage have either many intermediate drusens or more larger ones. Often they notice a blurry spot in their central vision and they may need more light for reading or other activities.
3. Advanced dry AMD
Besides drusens prescence at fundus, at this type of AMD there is damage of photoreceptors (neural cells which are sensitive to light) and supportive tissues at the central retinal region. These damages may cause a black spot at the center of vision. Over time, this black spot may become bigger and darker, as many patients mention difficulty in recognizing faces.
In case of vision loss due to dry AMD in one eye, patients may not observe problems in overall vision. If the other eye is not affected, patients are able to read, drive and distinguish details. Patients may mention changes when AMD affects both eyes. If someone perceive blurry vision, he should contact to an ophthalmologist for a comprehensive eye exam, which will include fundoscopy.
Dry type of AMD is more common. If we observe the case of intermediate and advanced AMD, more than 85% of patients are affected by dry AMD. However, if we observe and examine only the advanced dry AMD, about 2/3 of the patients may be affected by wet AMD. The significant vision loss usually occurs in patients who suffer from advanced AMD. So, it's obvious that wet AMD is responsible for vision loss much more than dry AMD.
Transformation of dry Age Related Macular Degeneration to wet type
The majority of patients who suffer from wet AMD, have dry type initially. Dry type of AMD may progress and provoke vision loss, without being transformed to wet AMD. However, dry AMD may be transformed suddenly to wet type, even at initial stages of the disease. Unfortunately, we cannot say for sure, if the dry type of AMD can be transformed to wet type and when this may happen.
Dry or wet advanced type of Age Related Macular Degeneration
Wet type of AMD is considered an advanced stage of AMD anyway. In general, wet AMD and advanced dry AMD are advanced stages of the disease. Vision loss may occur in both types of AMD. In the majority of cases only advanced stage of AMD may cause vision loss. Patients who suffer from advanced AMD in one eye, are in high risk of developing advanced AMD also in the other eye.
Risk factors for developing Age Related Macular Degeneration
The most important risk factor is the advanced age. Even though AMD may appear in the middle age, many studies have shown that people over 60 yo, are at higher risk, in relation to other age groups. For example, results from a comprehensive study have shown that the risk of developing AMD at the middle age is 2%, while this risk reaches 30% at the age over 75 yo.Other risk factors are:
• Smoking
• Obesity: Recent studies have shown that obesity may increase the risk of developing the initial stages to advanced stages of the disease.
• Race: White race presents greater risk of vision loss.
• Family history: People who have first-degree relatives who suffer from AMD are at higher risk.
• Sex: Women are at greater risk of developing AMD.
Life style which may reduce the risk of developing Age Related Macular Degeneration
• Healthy diet with lots of green vegetables and fish.
• Stop smoking
• Keep blood pressure at normal levels
• Keep your weight at normal levels
• Exercise
Age Related Macular Degeneration Symptoms
Both types of AMD do not provoke pain.
Dry type:
The most common early symptom is blurry vision. As fewer cells in the macula function properly, patients have difficulty in distinguishing details such as faces, or words in a book. Usually this blurred vision is improved in bright light conditions. If the destruction of macular cells is expanded, patients may observe a black spot in their central vision, which over time is extended.
Wet type:
The common earliest symptom is that the straight lines seem to be wavy. This is a result of fluid accumulation, which is derived from the leakage of the pathological neovascularization. A central black spot is formed in wet type of AMD, leading to loss of central vision.
Age Related Macular Degeneration Diagnosis
The ophthalmologist may suspect AMD if the patient is over 60 yo, and mentions recent changes-irritations in his central vision. In order to examine these signs it is necessary to dilate the pupils of the eye, using eye drops. This examination is called fundoscopy and allow us examine the macula in detail.
The AMD is diagnosed during comprehensive eye exam which includes:
Visual Acuity test: How well can a patient see the numbers which are displayed on a screen table.
Fundoscopy: The pupils are dilated using drops and the ophthalmologist uses a special magnifying lens to examine the whole macula, the optic nerve and the retina in general. After the examination and for the next few hours the near vision may remain blurry due to the dilation.
In addition, your ophthalmologist may request further tests for better condition's assessment of your eyes. During the examination, Amsler grid test can be used. The Amsler grid test is a small card which includes small squares like chessboard. Each eye is tested separately and is asked from the patient to focus on a central spot, while observing the straight lines. If the lines become wavy or if some boxes are missing from the network, we may assume the presence of AMD.
You may print your own Amsler grid test and use it at home!
Another useful special examination which is used for AMD diagnosis is fluorescein angiography. Through intravenous injection we use a specific dye and then we can photograph the blood circulation of the fundus. Thus, the ophthalmologist may see any blood vessels leakage. A similar examination which uses another type of dye is called Indocyanine Green Angiography or (ICG Angiography). In addition a non-invasive popular technique which gives us useful results in some seconds about AMD’s diagnosis is called Optical Coherence Tomography (OCT).
Wet Age Related Macular Degeneration treatment
The wet type of AMD may be treated by thermal laser photocoagulation, photodynamic therapy, or by intravitreal injections. Unfortunately, the disease may develop again despite the treatment.
• Thermal laser
This therapy treatment uses a thermal laser to destroy the abnormal blood vessels. However, at the same time, normal retinal tissue is also destroyed, because it is located above the pathological vessels. Thus, this treatment is now used very seldom, and only in cases where the abnormal blood vessels are located away from the center of the retina.
• Photodynamic therapy
In this case, a drug called verteporfin is injected intravenous. Then through blood circulation, reaches the abnormal blood vessels. When these vessels absorb verteporfin, the ophthalmologist uses a special non-thermal laser at the fundus, using a special lens for 83 seconds. This special laser activates the drug, which decompresses the abnormal vessels. Photodynamic therapy destroys the abnormal blood vessels, while leaving intact the normal tissue, in contrast to thermal laser treatment. Photodynamic treatment reduces vision loss. However, the results are often temporary and sometimes treatment should be repeated.
• Injections
Nowadays, wet type of AMD is treated by new drugs which are applied through intravitreal injection. These drugs treat a factor called VEGF, which has been found to be responsible for the development of the abnormal blood vessels. The patient will need repeated injections even per month. The eye is anesthetized before each injection. The treatment may reduce the vision loss and in some cases even improves vision. Approved treatments are ranibizumab, bevacizumab and aflibercept.
Eylea (aflibercept) Age Related Macular Degeneration
Aflibercept is a pharmaceutical substance of the drug Eylea. This substance inhibits the activity of a group of factors, known as vascular endothelial growth factors (VEGF). In patients who suffer from wet type of AMD, when these factors are increased, new abnormal formation of blood vessels may happen in the eye. These new blood vessels can cause blood leakage and subsequent damage of the eye tissue, which is responsible for vision.
How Eylea is administered?
Patients with wet AMD are advisable to receive treatment with one injection per month for three (3) consecutive doses, then one injection every two (2) months. In any case, depending on the stage of macular degeneration, your doctor will tell you the frequency of drug administration. The continuity and frequency of treatment is determined by measurements of visual acuity and optical coherence tomography (OCT).
Dry Age Related Macular Degeneration treatment
When dry AMD reaches the advanced stage and causes central vision loss, there is no available treatment. However, when the disease is at an intermediate stage, there is a treatment option, which may reduce the risk of further progression of disease. This treatment is done by using food supplements (antioxidants).
Partial vision loss due to Age Related Macular Degeneration
Patients who have already lost some part of their vision due to AMD, should not be afraid to use their eyes for reading, watching TV, or doing other daily routine activities, as there is no probability of further vision loss. If their vision has been seriously reduced, they should contact their ophthalmologist, in order to be informed about the vision-low aids, such as for example special lenses and telescopes.


