Diabetic Macular Oedema (DMO) is associated with diabetic retinopathy and may be appeared in any stage of the disease. This condition is one of the main macular diseases, among the age-related macular degeneration (AMD), central retinal vein occlusion (CRVO) and vitreomacular traction (VMT). According to the Greek vitreoretinal company, more than 50.000 people are affected by a macular disease. In particular, 30% of diabetic patients, who have diabetes over 20 years will be affected by DMO. Unless the oedema does not be treated with drugs, these patients will soon have a vision decrease.
What is the Diabetic Macular Oedema (DMO)?
In case of diabetes, high glucose levels may lead to destruction of some blood vessels in retina. These vessels become weaker and may leak liquid or even be occluded. The accumulation of liquid between the retinal layers is called DMO. DMO is the most important cause of vision decrease in diabetic patients.
The disruption of the blood-retinal barrier leads to leakage of plasma components in the surrounding retina, leading to retinal oedema.
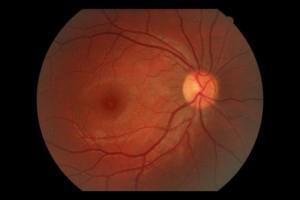 Normal Fundus
Normal Fundus
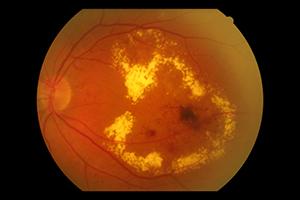 Fundus with Diabetic Macular Oedema
Fundus with Diabetic Macular Oedema
The decrease of vision can be ≥ 2 lines on the visual acuity chart in case of non-treatment administration in 50% of the patients.
The prevalence of visual impairment due to DMO depends on the type of diabetes and its duration.
In diabetic patients, the prevalence of the clinically significant macular oedema (CSMO) is about 6-10%.
Several studies have shown that 0.6% of general population is affected by CSMO.
Diabetic Macular Oedema (DMO) symptoms
• Vision decrease
• Paramorphopsia (distorted visual field)
• Contrast sensitivity decrease
• Photophobia
• Color vision problems
• Paracentral scotomas (black regions of visual field)
• Diplopia
• Floaters (sometimes)
The visual impairment due to DMO burdens the patient. For the patient the loss of independence can be a result of reduced ability of doing specific daily activities, like reading or driving leading to deterioration in his quality of life.
Risk factors
The diabetic Macular Oedema (DMO) may appear at any stage of the diabetic retinopathy and there are several risk factors that are associated with the condition and its prognosis.
• Increased levels of glycated hemoglobin (HbA1C)
• Hypertension
• Hyperlipidemia
• Diabetic nephropathy
• Smoking
What is the VEGF factor and how is associated with diabetic macular oedema (DMO)?
The continuous hyperglycemia in diabetic patients may affect the expression levels of several vasoactive factors, which in turn may contribute to structural and functional changes in DMO and diabetic retinopathy.
For instance, significantly increased levels of VEGF and interleukin -6 (IL-6) (factors which increase the vascular permeability) have been observed in the aqueous humor and in vitreous cavity in patients with DMO.
VEGF is a major mediator of increased retinal permeability. It may cause hyperpermeability of the blood-retinal barrier either directly or indirectly through some mechanisms. Increased expression of VEGF factors is caused by hypoxia on several retinal cells. Hypoxia is caused by vascular contraction in diabetic eyes.
Diabetic Macular Oedema (DMO) Clinical Diagnosis
Diabetic Macular Oedema can be diagnosed by fundoscopy (examination of fundus under dilated pupils), as well as by fundus photograph, where we can depict the macula and the optic nerve. A very useful tool is called Optical Coherence Tomography (OCT), where the operator (optometrist or ophthalmologist) can measure the thickness of the oedema and can detect also the presence of cysts between the retinal layers, any serous retinal detachment, the presence of epiretinal membrane and if there is blood between the retinal layers. With this technology, we can also compare the thickness of the oedema when the patient gets some treatment for the oedema.
 OCT with Normal Macula
OCT with Normal Macula
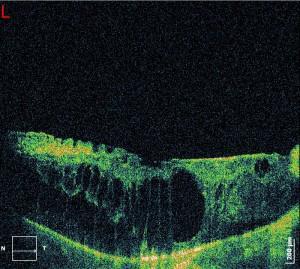 OCT with Diabetic Macular Oedema (DMO)
OCT with Diabetic Macular Oedema (DMO)
Diabetic macular Oedema treatment
The main treatment method of the diabetic macular oedema (DMO) is retinal photocoagulation by Argon laser. In cases of focal oedema, photocoagulation of microaneurisms is performed, whereas in cases of diffuse oedema, grid laser or modified grid laser is performed.
In addition, anti-VEGF factors are also promising according to many studies. Ranibizumab (Lucentis) is a small portion of a fully humanized monoclonal antibiotic that inhibits multiple forms of vascular endothelial growth factor (VEGF)-A.
The drug is administered by intravitreal injection under sterile conditions in the operating room by a surgeon ophthalmologist, who is trained in intravitreal injections.
We repeat the treatment once in a month, until the maximum visual acuity is achieved (stable visual acuity for three consecutive monthly assessments during the treatment with Lucentis). Therefore, if there is no improvement on visual acuity during the time of injections treatment, we don't recommend to the patient to continue the injections.
Thereafter, patients need to have a monthly appointment for visual acuity examination. The treatment can be repeated when there is a loss of visual acuity due to DMO. In this case the ophthalmologist may continue the annual injections, until the patients achieves again his visual acuity for three consecutive ophthalmological assessments.
The time interval between two doses should not be shorter than one month.
The latest news about treatment of diabetic macular oedema in diabetic patients.
Diabetic Retinopathy is a chronic progressive disorder of the retinal vascular system and is the most common microvascular complication of diabetes. The majority of patients who have diabetes for up to a decade, will develop diabetic retinopathy to some extent. At initial stages, diabetic retinopathy causes microaneurysms and hemorrhages. The white spots which appear in the retina also known as exudates, are caused due to ischemic occlusions located in the nerve fiber layer. The exudates can be observed through fundoscopy (examination of the retina through dilated pupils), as well as Optical Coherence Tomography (OCT).
The next and most advanced stage of retinopathy, which is called proliferative diabetic retinopathy is characterized by arterioles and venules occlusion and creation of a new vascular network in the optic disc, retina, iris and the angle of the anterior chamber.
Vitreous hemorrhage is a common complication of the productive diabetic retinopathy, which occurs as a result of blood leakage from new abnormal veins of the vitreous cavity.
Eylea (aflibercept) intravitreal injections treatment Diabetic Macular Edema.
Aflibercept is a pharmaceutical substance of the drug Eylea. This substance inhibits the activity of a group of factors, known as vascular endothelial growth factors (VEGF). Diabetic macular edema is formed due to diabetic changes in fundus. Specifically, there is leakage of fluid from blood vessels within the macula, which is responsible for good our central vision. When the macula is filled up with liquid, our central vision becomes blurred. Eylea has been demonstrated to stop the development of new abnormal blood vessels in the eye, which often exhibit liquid leakage or bleed. It can also stabilize or even improve vision in many cases.
How Eylea is administered?
Patients with diabetic macular edema can be treated with one (1) injection per day for five (5) consecutive doses, and then an injection every two (2) months is administered. Your ophthalmologist, depending on the stage of the disease identifies the frequency of the treatment. Based on re-evaluation, which is carried out by measuring visual acuity and also through optical coherence tomography (OCT) , where the thickness of the edema is measured and compared, your doctor can give you the proper instructions about treatment with intravitreal Eylea injection.

