A macular hole is a retinal break commonly involving the fovea. Patients with macular holes typically present over the age of 60 and females are more frequently affected.
A careful history should be obtained to investigate for any of the risk factors mentioned above. Different findings can be observed depending the stage of the macular hole. Residual cortical vitreous, retinal glial, and retinal pigment epithelial cells are often found on the retinal surface. They are thought to cause tangential traction on the fovea. Cystoid edema in the outer plexiform and inner nuclear layers and thinning of the photoreceptor layer can also be observed.
It has been hypothesized that macular holes are caused by tangential traction as well as anterior posterior traction of the posterior hyaloids on the parafovea. Macular holes are noted as a complication of a posterior vitreous detachment (PVD) at its earliest stages.
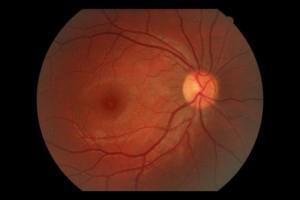 Natural Fundus
Natural Fundus  Fundus with macular hole
Fundus with macular hole
 Full Thickness Macular Hole
Full Thickness Macular Hole  Full Thickness Macular Hole with Retinal Detachment
Full Thickness Macular Hole with Retinal Detachment





