Diabetes mellitus is a metabolic disease which is characterized by increase of blood sugar concentration and wrong glucose metabolism, either as a result of decreased insulin secretion, or due to reduction of the sensitivity of body cells to insulin.
 Diabetic Retinopathy
Diabetic Retinopathy
According to the World Health Organization, in 2006, patients with diabetes exceeded 170 million worldwide, a figure which is expected to be double by 2030, as the incidence of diabetes increases rapidly.
It is estimated that in Greece, the 5.9% of the general population suffers from diabetes. The disease may cause a range of serious complications in adults and children, such as cardiovascular disease, chronic renal failure, nerve damage and eye problems.
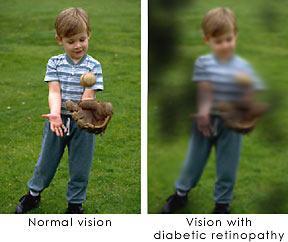
How diabetes influences our vision?
Patients with diabetes are more likely to develop eye problems, such as cataracts or glaucoma. However, the main sight’s threat from diabetes is the attack of retina. This condition is known as diabetic retinopathy and occurs in the majority of patients after 10-15 years of the disease.
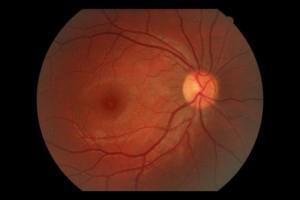 Normal Fundus
Normal Fundus
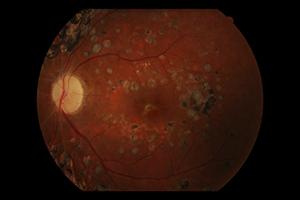
 Fundus with Diabetic Retinopathy
Fundus with Diabetic Retinopathy
 Hemorrhage in Diabetic
Hemorrhage in Diabetic
Retinopathy
The earliest stage of the disease is known as diabetic retinopathy’s substrate. At this stage, the arteries in the retina are weakened and leak, thus forming small hemorrhages. The vessels which leak, often lead to edema and vision decrease.
The next stage of the disease is known as proliferative diabetic retinopathy. At this stage, problems in the circulatory system of the retina cause some areas to become ischemic. New, fragile vessels grow, in order to help the circulatory system to maintain adequate oxygen vessels within the retina (neovascularization). Unfortunately, these weakened blood vessels bleed easily and the blood may leak into the retina and vitreous, causing blurring, floaters and vision’s decrease.
In more advanced stages of the disease, continuous, abnormal increase of neovascularization, as well as scarring tissue, may cause serious problems, such as retinal detachment due to traction and glaucoma.
 Diabetic Retinopathy
Diabetic Retinopathy
Symptoms of Diabetic Retinopathy
The influence of diabetic retinopathy on patient’s vision varies, depending on the stage of the disease. However, there are some common symptoms such as:
- Blurred vision (this is associated with blood glucose vessels)
- Floaters and flashes
- Sudden decrease or loss of vision
Testing and Diagnosis
People who suffer from diabetes need regular eye tests, so that vision problems can be detected and treated as early as possible. Most diabetic patients are examined by a diabetologist or endocrinologist who then works together with an ophthalmologist.
The diagnosis of diabetic retinopathy is decided after a detailed examination of the retina fundus. Usually the patients with diabetic retinopathy are referred to ophthalmologists-vitreoretinal surgeons who are specialized in the treatment of the disease.
{slider Treatment of Diabetic Retinopathy}
Diabetic Retinopathy can be treated by various ways, depending on the stage of the disease and the existed problem on the retina. The patient will be submitted in a series of eye examinations, in order to determine the disease’s progress, such as fluoroangiography, fundus photography, optical coherence tomography (OCT) and fundus check using ultrasound (when it is needed).
 Laser for Diabetic Retinopathy
Laser for Diabetic Retinopathy
In early stages of the disease, panretinal photocoagulation using Argon Laser can be a valuable option for treatment. Using Argon Laser the surgeon-ophthalmologist uses the laser to destroy the oxygen-deprived retinal tissue around the central retina. This treatment creates blind spots in the peripheral vision and avoids the continuous increase fragile vessels’ neovascularization and seals any leakage. The goal is to inhibit disease’s progression.
The vitrectomy is a surgical procedure, which is usually applied in patients with vitreous hemorrhage (vitreous is the transparent substance, like a gel, that fills the inner cavity of the eye). During vitrectomy, the surgeon-ophthalmologist carefully removes the blood, as well as the vitreous from the eye and replaces it with saline. Simultaneously, the surgeon may separate and cut several regions of vitreous that are tightly stucked on the retina and create traction to him with very delicately tools. (These tractions may create further hemorrhages or cracks on the retina, as well as retinal detachment).
Patients with diabetes are at higher risk of retinal cracks and retinal detachment. Cracks are often sealed, during laser surgery, while the detachment requires surgery, in order to attach the retina back to its initial position, in the back of the eye.
Prevention
Researchers have found that patients who are able to maintain appropriate blood glucose levels have fewer eye problems, than those who do not proceed for their regular check of their situation. Diet and exercise play an important role in the overall health of diabetic patients and the complications of their vision are greatly reduced by regular eye examinations.
Many problems can be dealt with much more success if are diagnosed early!

