Epiretinal membrane is a disease of the eye in response to changes in the vitreous humor or more rarely, diabetes. It is also called macular pucker.
Sometimes, as a result of immune system response to protect the retina, cells converge in the macular area as the vitreous ages and pulls away in posterior vitreous detachment (PVD). PVD can create minor damage to the retina, stimulating exudate, inflammation, and leucocyte response. These cells can form a transparent layer gradually and, like all scar tissue, tighten to create tension on the retina which may bulge and pucker (e.g. macular pucker), or even cause swelling or macular edema. Often this results in distortions of vision that are clearly visible as bowing when looking at lines on chart paper (or an Amsler grid) within the macular area, or central 1.0 degree of visual arc. Confirmation of the problem, as well as the display of its size, is done using the Optical Coherence Tomography (OCT).
Usually it occurs in one eye first, and may cause binocular diplopia or double vision if the image from one eye is too different from the image of the other eye. The distortions can make objects look different in size (usually larger = macropsia), especially in the central portion of the visual field, creating a localized or field dependent aniseikonia that cannot be fully corrected optically with glasses. Partial correction often improves the binocular vision considerably though. In the young (under 50 years of age), these cells occasionally pull free and disintegrate on their own; but in the majority of sufferers (over 60 years of age) the condition is permanent. The underlying photoreceptor cells, rod cells and cone cells, are usually not damaged unless the membrane becomes quite thick and hard; so usually there is no macular degeneration.
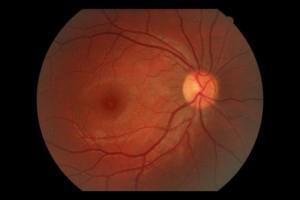
Natural Fundus
 Fundus with Epiretinal Membrane
Fundus with Epiretinal Membrane
Symptoms of Epiretinal Membrane
- Blurred vision
- Diplopia
- Distorted vision (straight lines might seem wavy)
Surgery for epiretinal membrane
Surgeons can remove or peel the membrane through the sclera and improve vision by 2 or more Snellen lines. Usually the vitreous is replaced at the same time with clear fluid, in a vitrectomy. Surgery is not usually recommended unless the distortions are severe enough to interfere with daily living, since there are the usual hazards of surgery, infections, and a possibility of retinal detachment. More common complications are high intraocular pressure, bleeding in the eye, and cataracts, which are the most frequent complication of vitrectomy surgery. Many patients will develop a cataract within the first few years after surgery. In fact, the visual distortions and diplopia created by cataracts may sometimes be confused with epiretinal membrane.
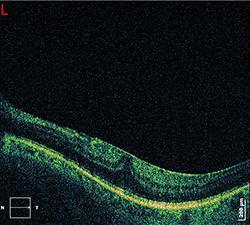
 Natural OCT
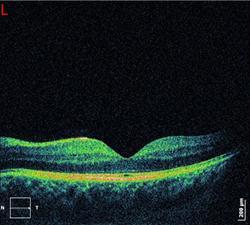
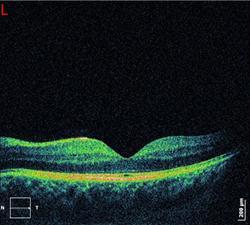
Natural OCT  OCT with Epiretinal Membrane
OCT with Epiretinal Membrane
 OCT with Epiretinal Membrane
OCT with Epiretinal Membrane 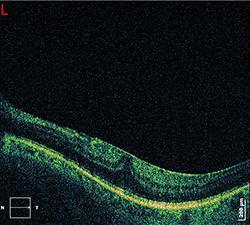 OCT with Epiretinal Membrane
OCT with Epiretinal Membrane
Prevention of Epiretinal membrane
There is no good evidence for any preventive actions, since it appears this is a natural response to aging changes in the vitreous. Posterior vitreous detachment (PVD) has been estimated to occur in over 75 per cent of the population over age 65, that PVD is essentially a harmless condition (although with some disturbing symptoms), and that it does not normally threaten sight. However, since epiretinal membrane appears to be a protective response to PVD, where inflamation, exudative fluid, and scar tissue is formed, it is possible that NSAIDs may reduce the inflammation response. Usually there are flashing light experiences and the emergence of floaters in the eye that herald changes in the vitreous before the epiretinal membrane forms.
Complications
Eye infection is a very serious complication that needs serious treatment. There is also a small risk of retinal detachment the first months after the surgery.
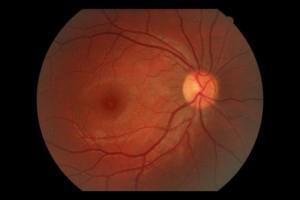
 Fundus with Epiretinal Membrane
Fundus with Epiretinal Membrane